The Heart–Brain Connection and What It Means for Heart Rate Variability (HRV)
A look at a few recent scientific articles exploring heart rate modulation via brain stimulation and oxytocin.
Where does Heart Rate Variability (HRV) come from?
We often say that HRV reflects vagal tone, but that is not entirely correct. HRV arises from the interaction of several systems: baroreflex function, parasympathetic modulation, hormonal and neurochemical regulation, and mechanical influences on the heart and blood vessels. HRV cannot be equated directly with vagal tone and can easily decouple from it, for example when measured continuously.
HRV is an indirect manifestation of oscillations in cardiovascular control and reflects the behavior of a tightly coupled network more than a single pathway. Still, under the right conditions (measured intentionally at rest, with stable/relaxed breathing, consistent posture, and avoiding artifacts such as swallowing, yawning, talking, or ectopics), HRV remains the most accessible and reliable proxy of cardiac vagal modulation we have.
Recent work on how the brain and heart communicate provides additional evidence for the interpretation above and shows how deeply integrated the brain and heart are. Let’s get to it.
Modulating Heart Rate with Transcranial Stimulation
I was recently in contact with Martijn Arns, PhD, who is an applied neuroscientist and entrepreneur with a longstanding focus on brain stimulation, neurofeedback/BCI, and medtech innovation (and a runner!). Martijn brought to my attention two recent studies he has co-authored, which you can find here and here. The two studies by Dijkstra et al. and colleagues used transcranial magnetic stimulation to explore how stimulating parts of the prefrontal cortex affects heart rate.
The results are very interesting: rhythmic cortical stimulation produced rhythmic cardiac decelerations at the same frequency, around 0.1 Hz, the same range typically seen in respiratory sinus arrhythmia:
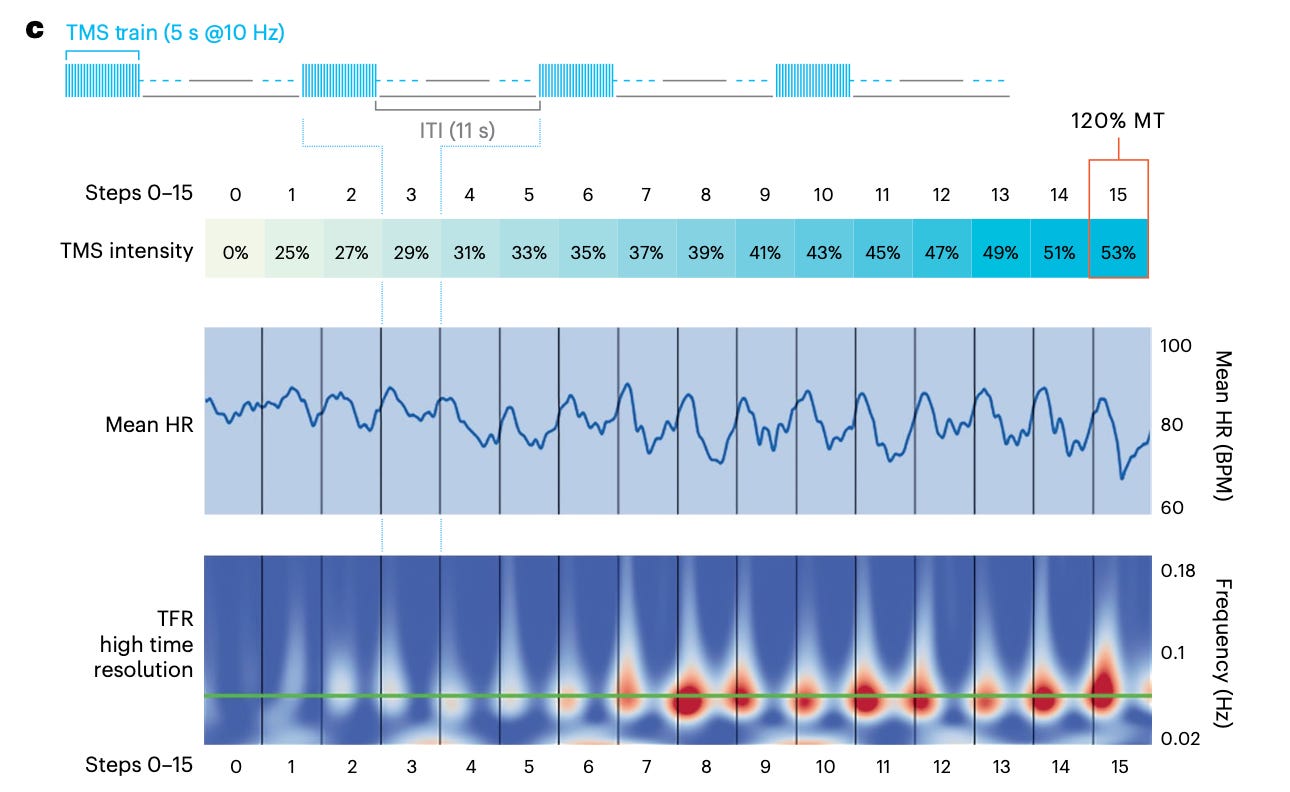
Stimulating brain regions can modulate heart activity in a predictable, frequency-defined way. These findings suggest that higher brain centers regulate autonomic output through vagal pathways. I found it particularly interesting that this type of stimulation can also completely dissociate from respiratory sinus arrhythmia, or the natural heart rate changes we all experience because of respiration (i.e., heart rate increasing when breathing in, and decreasing when breathing out). Through brain stimulation, this pattern can be completely overridden.
This work gives us another mechanistic foundation for why HRV changes with emotional and cognitive states, as the same cortical regions that regulate mood can also influence vagal outflow.
The Role of Oxytocin
Another recent paper published in Nature Neuroscience (Buron et. al., see here) adds another layer, looking at the role of oxytocin, a neuropeptide made in the hypothalamus and known to help regulate social behavior, stress responses, and autonomic functions.
In their work, the authors identified a hypothalamus–brainstem neuronal pathway through which oxytocin amplifies HRV during calming behavior / recovery from stress (in rodents!). In particular, Buron and colleagues mapped a hypothalamus–brainstem pathway from oxytocin neurons to vagal motor nuclei, first recording neural activity during calming behavior and recovery from stress, and then selectively activating or inhibiting oxytocin neurons. When doing so, HRV increased and respiratory sinus arrhythmia was amplified during recovery.
As the authors mention, relaxation and positive socio-emotional states can amplify HRV (respiratory sinus arrhythmia is what they looked at here). This study provides another mechanistic foundation of the link between the brain and the heart, and how neurochemical modulation in the brain can shape vagal output as captured by HRV.
Wrap up
Together, these papers support the idea that HRV is a proxy for vagal modulation. They confirm that brain regions and neurochemical systems influence cardiac activity through vagal pathways, while reminding us that HRV reflects the output of an integrated system, not a single source.
When measured under the right conditions (short, resting, morning assessments with stable breathing - ideally measured using an ECG - is how I’d recommend it), HRV remains a reliable window into how our nervous system responds to training and life stressors.
I found these papers really interesting and I’m looking forward to following further developments from these research groups. I hope there was something interesting in there for you as well!
Personal Coaching for Runners
If you are interested in working with me, please learn more here, and fill in the athlete intake form, here.
How to Show Your Support
No paywalls here. All my content is and will remain free.
As a HRV4Training user, the best way to help is to sign up for HRV4Training Pro.
Thank you for supporting my work.
Marco holds a PhD cum laude in applied machine learning, a M.Sc. cum laude in computer science engineering, and a M.Sc. cum laude in human movement sciences and high-performance coaching. He is a certified ultrarunning coach.
Marco has published more than 50 papers and patents at the intersection between physiology, health, technology, and human performance.
He is co-founder of HRV4Training, advisor at Oura, guest lecturer at VU Amsterdam, and editor for IEEE Pervasive Computing Magazine. He loves running.
Social:
Personal Substack
Instagram



